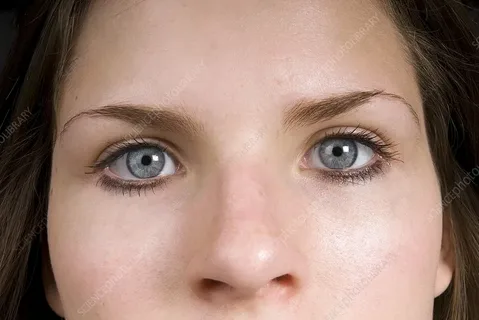
A small, constricted pupil might not seem alarming at first glance, but when it appears after an injury to the eye, it can signal something serious. A pinpoint pupil—defined as a pupil less than 2 mm in diameter—may result from trauma, surgical complications, or damage to the muscles and nerves that control the eye. Whether you’ve sustained a blow to the eye, undergone a recent operation, or are caring for someone after an accident, understanding what pinpoint pupils indicate in the context of eye injuries can make all the difference.
Understanding Pinpoint Pupils
A pinpoint pupil is typically unresponsive or minimally reactive to changes in light. While it’s sometimes caused by drugs or neurological conditions, eye trauma is another key factor. In the context of an injury, the pupil’s inability to dilate may reflect direct physical damage or a deeper neurological issue involving the brainstem or cranial nerves.
When one or both pinpoint pupils appear after an injury, it should never be ignored—it’s often your body’s way of sounding an alarm.
How Eye Injuries Lead to Pinpoint Pupils
Let’s break down the main mechanisms through which trauma can lead to a pinpoint pupil:
1. Iris Sphincter Muscle Damage
The iris contains muscles that control how much light enters the eye. Trauma, such as a sharp object entering the eye or blunt force impact, can damage the sphincter muscles responsible for dilation. When these muscles are injured, the pupil may remain tightly constricted—essentially stuck in the “closed” position.
2. Nerve Damage
The third cranial nerve (oculomotor nerve) carries signals that help regulate pupil size. Trauma affecting the nerve—either directly through injury or indirectly via swelling or bleeding inside the skull—can interfere with its function. In rare cases, this may result in a pinpoint pupil, though nerve damage more often causes pupil dilation.
3. Post-Surgical Response
Eye surgeries such as cataract removal, glaucoma treatment, or even cosmetic procedures near the eyelid can impact the delicate muscles around the iris. Some surgeries involve intentional constriction of the pupil to protect the inner structures of the eye during recovery. In these cases, a pinpoint pupil may be a planned but temporary outcome.
4. Sympathetic Chain Injury
A severe neck or upper chest injury may impact the sympathetic nerve fibers that influence pupil dilation. This can lead to Horner’s syndrome, which often presents with a pinpoint pupil, drooping eyelid, and reduced facial sweating on one side.
When Is It Serious?
Not every pinpoint pupil caused by trauma is a medical emergency, but certain warning signs should prompt immediate evaluation:
- Loss of vision or sudden visual changes
- Pain in or around the eye
- Bleeding from the eye or surrounding structures
- Unequal pupil size (anisocoria) following injury
- Drooping eyelid or facial weakness
- History of head trauma or concussion
These symptoms may indicate deeper damage—such as intraocular bleeding, orbital fracture, or even brain injury—and should be evaluated by an ophthalmologist or emergency doctor without delay.
Diagnostic Tools
To determine the cause of a pinpoint pupil after injury, doctors use a variety of tools:
- Penlight Examination – To assess pupil reactivity to light and compare both eyes.
- Slit Lamp Exam – Provides a detailed view of the cornea, lens, and iris to detect internal injuries or foreign bodies.
- Ophthalmoscopy – Examines the retina and optic nerve for trauma-related damage.
- CT Scan or MRI – If head trauma is suspected, imaging can identify fractures, hemorrhages, or brain swelling.
- Neurological Exam – To rule out cranial nerve damage or brainstem involvement.
Treatment Options
Treatment depends on the underlying cause. If the pinpoint pupil is due to iris muscle damage, the pupil may never fully regain its normal function, though it may not affect vision significantly. In other cases:
- Medication such as atropine may be used to dilate the pupil temporarily.
- Surgery may be necessary to repair structural damage or relieve pressure inside the eye.
- Observation is appropriate when the pupil change is temporary or a known result of recent surgery.
In trauma-related cases involving the brain or nerves, management may include steroids, neuroprotective therapies, or even neurosurgical intervention.
Prevention and Long-Term Care
To reduce the risk of developing a pinpoint pupil from eye trauma, always wear protective eyewear during sports, hazardous work, or activities involving sharp tools. Regular eye exams are essential, especially if you’ve had prior eye injuries or surgeries. If a pinpoint pupil persists, follow up with a specialist to monitor for secondary complications such as light sensitivity or focus issues.
Conclusion
Eye injuries can lead to many unexpected symptoms, and a pinpoint pupil is one of the most important to recognize. Whether the result of blunt force, surgery, or neurological disruption, a pinpoint pupil is more than a cosmetic concern—it’s a sign that something deeper may be wrong. Understanding the causes and seeking prompt medical attention can preserve vision and, in some cases, even save lives.
read also this article